Pregnancy and postpartum aren’t just life chapters—they’re a total body, mind, and identity transformation. From the first flutter in your belly to the exhausting newborn nights, this journey is as emotional as it is physical.
But while everyone focuses on pregnancy, what happens after birth is just as crucial—and often ignored.
The healing, rebuilding period (the “fourth trimester”) is a critical time of healing, hormonal shifts, and self-rediscovery. Yet no one hands you a recovery manual at the hospital.
- How do you heal from birth—whether vaginal or C-section?
- What’s normal vs. a red flag in postpartum bleeding?
- When will you feel like yourself again?
This guide covers everything you need to know – from trimester-by-trimester changes and how to cope with them, to realistic postpartum recovery timelines showing what really happens after birth, plus essential mental health strategies, nutrition advice, and fitness approaches to help you regain strength.
Whether you’re expecting your first or navigating newborn life, this is your no-fluff, evidence-backed roadmap to thriving, not just surviving.
Pregnancy & Postpartum Wellness Summary / Overview
Pregnancy and postpartum wellness involves prioritizing a mother’s physical, mental, and emotional health through nourishing nutrition, adequate rest, and support systems. Key strategies include managing postpartum pain, monitoring mental health for depression/anxiety, and gentle, gradual rehabilitation, such as pelvic floor exercises. Essential care includes seeking social support, accepting help, and attending all postpartum checkups to ensure recovery.
What Is Postpartum Wellness?

Postpartum wellness is the holistic physical, mental, and emotional recovery of a mother after childbirth, focusing on healing, hormonal balance, and emotional health. It involves proper nutrition, gradual exercise, and managing conditions like fatigue or anxiety to ensure long-term health, often prioritizing self-care for the mother amid the demands of a new baby.
You’ve just performed a miracle—bringing life into the world. Now what?
Postpartum wellness isn’t just a buzzword; it’s the complete physical, mental, and emotional recovery of a mother after childbirth. Think of it as your body’s extraordinary journey back to strength, your mind’s adjustment to a new identity, and your heart learning to navigate a love like no other. While your baby’s health is, of course, central, your well-being is equally – if not more – critical. Why? Because a healthy, supported mom is the best foundation for a thriving family.
But let’s be honest, the postpartum period, often called the “fourth trimester,” comes with its own unique set of challenges that can catch many new mothers by surprise:
- The Body’s Comeback Tour: Your body has just performed a miracle! Now, it needs time and care to heal. This involves navigating everything from pelvic floor issues (hello, jumping jacks might feel different!) to persistent fatigue that sleep just doesn’t seem to touch, and managing various postpartum pains.
- A Rollercoaster of Emotions: Imagine a symphony of hormones, sleep deprivation, and the immense pressure of new parenthood. This can often lead to a whirlwind of feelings. It’s why many mothers experience postpartum depression (PPD), anxiety, and even profound feelings of isolation. Your mental and emotional health isn’t just “feelings”; it’s a vital part of your overall recovery.
- Fueling Your New Superpower: Recovering from pregnancy and childbirth is like running a marathon – your body needs proper fuel! Focusing on solid nutrition, consistent hydration, and gradually reintroducing physical rehabilitation is key to regaining lost strength and energy.
Mothers need robust support during this time. The World Health Organization (WHO)even emphasizes that postpartum care is critical for reducing maternal health complications and improving long-term well-being. Yet, a surprising truth remains: many new mothers receive very little structured support after their initial six-week checkup. They’re often left to navigate this complex, beautiful, and sometimes overwhelming period largely on their own.
Pregnancy in 3 Trimesters
Understanding what happens during each stage of pregnancy can make the journey smoother. We’ll look at the amazing fetal growth and changes in your body, often described in pregnancy week by week.
Second Trimester
Third Trimester
The first trimester of pregnancy spans from week 1 through the end of week 13, marking a period of rapid development for the embryo/fetus and significant hormonal changes for the body. Key symptoms include extreme fatigue, nausea (morning sickness), breast tenderness, frequent urination, and mood swings. It is a critical period for fetal organ development.
Check out our complete and informative detailed guide about about What to Expect in First Trimester of Pregnancy: 101 Complete Guide & Tips.
The second trimester (weeks 14–27) is often considered the most comfortable, featuring increased energy, reduced morning sickness, and noticeable baby movements (quickening) around week 20.
The fetus grows rapidly, developing facial features, hair, and a 1–2 lb weight. Common symptoms include skin changes, backaches, and Braxton Hicks contractions.
Check out our complete and informative detailed guide about about Second Trimester of Pregnancy: What to Expect (13–27)
The third trimester, spanning from week 28 to birth (typically week 40), is the final, often uncomfortable stage of pregnancy focused on rapid fetal growth and preparation for labor. The baby gains significant weight, develops fat, matures lungs, and usually turns head-down.
Common symptoms include Braxton Hicks contractions, fatigue, backaches, and frequent urination. Check out our complete and informative detailed guide about about Everything y about the Third Trimester of Pregnancy (weeks 28 to 40)
Prenatal Care and Wellness Habits
Taking good care of yourself during pregnancy isn’t just good for you; it’s great for your baby, too. Focusing on pregnancy and postpartum wellness means building healthy habits.
- Physical Wellness: Yoga, Walking, Stretching: Staying active with pregnancy-safe exercises like walking, swimming, and prenatal yoga benefits both your body and mind. Gentle stretching can help with common aches. Exercise boosts blood flow and can help with inflammation reduction, making you feel better overall. [ACOG guidelines on exercise during pregnancy]
- Nutritional Needs & Hydration: Eating well is super important. Focus on a balanced diet with plenty of fruits, vegetables, lean proteins, and whole grains. Staying hydrated by drinking lots of water is also key. Your doctor will likely recommend prenatal vitamins to ensure you’re getting enough essential nutrients like folic acid and iron. Foods rich in magnesium and fiber are great for energy and digestion, while omega-3 fatty acids are vital for your baby’s brain development.
- Rest and Sleep: Don’t underestimate the power of rest. Your body is working hard, and getting enough sleep helps you cope with fatigue and supports your baby’s growth. Aim for consistent sleep cycles and create a comfortable sleep environment.
Managing Common Pregnancy
- Managing Common Pregnancy Symptoms: Pregnancy comes with its own set of unique symptoms. Here’s how to manage some common ones.
- Morning Sickness & Nausea Relief: Feeling queasy? Small, frequent meals, bland foods, and avoiding strong smells can help. Ginger supplements can also be very effective for nausea relief. Stay hydrated.
- Pregnancy Back Pain Relief: As your bump grows, back pain is common. Good posture, supportive shoes, and gentle stretches can make a big difference. A body pillow can provide support while sleeping. Sometimes, a compression belt recommended by your doctor can offer relief.
- Managing Pregnancy Fatigue: Fatigue is especially common in the first and third trimesters. Listen to your body and rest when you need to. Eating iron-rich foods and ensuring good hydration can help. Discuss any severe fatigue with your doctor, as it could be a sign of low iron. Magnesium intake can also sometimes help with energy levels.
Understanding Special Pregnancy Conditions
Sometimes, conditions can arise during pregnancy that need special attention.
- Gestational Diabetes Diet: Gestational diabetes is when a woman develops high blood sugar during pregnancy. It’s usually diagnosed with a glucose tolerance test. Managing it often involves a specific gestational diabetes diet focused on balancing carbohydrates, proteins, and fats to help with blood sugar regulation. In some cases, insulin might be needed. [CDC info on Gestational Diabetes]
- High-Risk Pregnancy Signs: A high-risk pregnancy means there might be a higher chance of health problems for the mother or baby. Signs can include certain pre-existing conditions, age, or complications that develop during pregnancy. Your doctor will monitor you closely for any fetal risk or other issues. It’s important to follow all hospital policies and the doctor’s advice if your pregnancy is considered high-risk.
- Vitamin K Shot Pros and Cons: The vitamin K shot is often given to newborns shortly after birth to prevent a rare but serious bleeding disorder. It’s a standard practice with significant benefits, though parents can discuss its pros and cons with their healthcare provider. [ACOG statement on Vitamin K]
Birth & Recovery: What Happens After Delivery
Congratulations, your baby is here! Now, it’s time for postpartum recovery tips and healing.

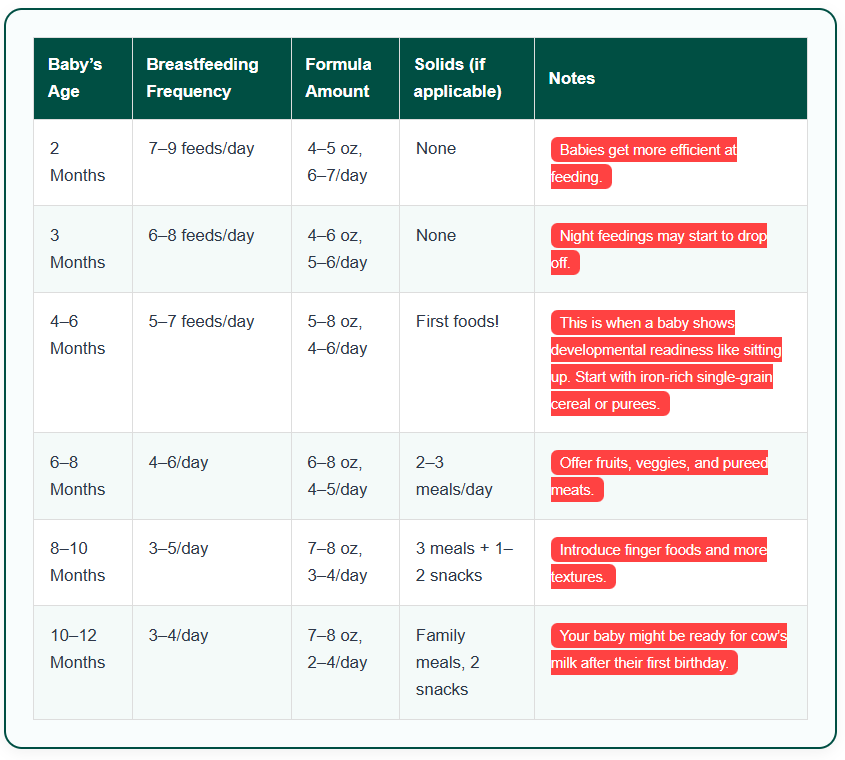
|
|
| |||
|---|---|---|---|---|---|
|
|
| |||
|
|
| |||
|
|
| |||
|
|
| |||
|
|
| |||
|
|
| |||
|
|
|
Both types of birth can involve stitches. For vaginal births, you might have stitches from a tear or episiotomy. A Sitz bath can be very soothing for perineal soreness. For c-sections, proper surgical wound care is essential to prevent infection.
The uterus goes through uterine involution, shrinking back to its normal size, which causes cramps, especially when breastfeeding. You’ll also experience a significant hormone crash as pregnancy hormones leave your system. Understanding wound healing stages is key.
Breastfeeding, Nutrition & Hormonal Rebalancing
Breastfeeding is a natural way to nourish your baby, but it can come with its own set of challenges.
Latch Techniques + Common Problems
A good breastfeeding latch is crucial for successful feeding and preventing nipple pain. A lactation consultant can offer invaluable support for increasing milk supply, correcting latching, and troubleshooting common problems like engorgement or mastitis. Your baby’s natural suck reflex is strong, but sometimes they need a little guidance.
Diet, Hydration, Galactagogues
Eating a nutritious breastfeeding diet, essential,s and staying well-hydrated are important for milk production. Some mothers find that certain foods or herbs, called galactagogues (like fenugreek), can help increase milk supply, but always consult with your doctor or lactation consultant.
Lanolin cream can be soothing for sore nipples. The hormone prolactin levels play a key role in milk production, and milk letdown is the reflex that releases milk from your breasts.
Postpartum Healing: Rebuilding Strength, Identity & Emotional Well-being
Your body has done an incredible job, and now it’s time to gently rebuild strength. This also involves embracing your new identity as a mother. The emotional side of postpartum can be just as intense as the physical.
Distinguish Between PPD, Anxiety, Baby Blues
It’s common to experience the “baby blues” in the first few weeks after birth – feeling teary, irritable, or anxious. This usually passes. However, baby blues vs postpartum depression is an important distinction. Postpartum depression signs are more severe and last longer, affecting your ability to function. Postpartum anxiety is also common. The intense hormonal shifts involving oxytocin, prolactin, and cortisol can play a role in these feelings.
Address Hormone Role, Sleep, Support Networks
Sleep deprivation, hormonal changes, and the huge responsibility of a new baby can all impact your mental health. Don’t suffer in silence. Talking to your partner, friends, family, or joining a support group can help. If you’re struggling, seeking therapy or professional help is a sign of strength. Focus on your self-worth and try to let go of maternal guilt. Building emotional resilience takes time and support.
Pelvic Floor Exercises Postpartum
Your pelvic floor muscles support your bladder, bowel, and uterus, and they need attention after birth. Gentle pelvic floor exercises postpartum (Kegels) are crucial for bladder control and overall core strength. A pelvic floor therapist can provide personalized guidance, especially if you experience issues like diastasis recti (separation of abdominal muscles).
Postpartum Body Strengthening & Postpartum Pelvic Care Tips
Start with gentle movements and gradually increase intensity. Focus on core stabilization exercises. It’s not about “bouncing back” but about patiently regaining strength. Connecting with your body and appreciating what it has achieved is an important part of your postpartum body image support. Working on your posture also helps.
Conclusion
This incredible journey from pregnancy through postpartum isn’t just a physical transition; it’s a profound transformation of your entire being. You’ve navigated immense changes, shown incredible resilience, and discovered a strength you may not have known you possessed.
Remember, focusing on your postpartum wellness isn’t selfish; it’s essential. It’s about honoring the amazing work your body has done, nurturing your mental and emotional health, and recognizing that a well-supported mother is the heart of a thriving family. Give yourself the same compassion and care you give your little one. Lean on your support system, seek help when needed, and celebrate every small victory. You are strong, capable, and truly amazing.



[…] often around the abdomen, hips, and thighs, are the primary targets for liposuction. You can check The Ultimate Guide to Pregnancy and Postpartum Wellness: From Bump to Baby Recovery, offering a deep dive into one specific aspect of postpartum body […]
[…] After birth pelvic exercise is a key part of healing, not just for your body, but for your mind, too. Taking care of yourself after bringing a new life into the world is essential. For a complete overview of recovery and overall health, you can explore our guide on pregnancy and postpartum wellness. […]
[…] So, you just found out you’re pregnant. Congrats! And also… wow, what a ride, right? Welcome to the first trimester of pregnancy, a time that’s basically a wild mix of excitement, hormones, and a whole lot of weird stuff happening to your body. Learning about first trimester symptoms is like getting a cheat sheet for the next few months. We’ll walk through exactly what to expect in first trimester so you can feel confident and prepared. This is just one small part of your larger journey toward pregnancy and postpartum wellness. […]